In medical care, understanding the diverse world of wound dressings is paramount. As the first line of defense in healing, these vital products play a crucial role in ensuring effective and efficient recovery. In this comprehensive guide, we unveil the essential knowledge behind 11 distinct types of wound dressings.
Traditional Wound Dressings
Comprising materials like cotton or synthetic fibers in forms such as gauze, cotton pads, and bandages, these wound dressings, often termed inert dressings, play a crucial protective role.
Applications:
Suitable for various wounds, often used as the outermost layer of dressings.
Gauze directly protects wounds.
Moistening gauze with saline helps maintain wound moisture.
Combined with medications, they effectively deliver drugs to the wound.

Advantages:
Protection of the wound.
Absorption of a small amount of exudate.
Easily accessible materials at an affordable price.
Utilization for physical debridement, efficiently removing necrotic tissue.
Drawbacks:
Inert healing nature, quick-drying, early scabbing, hindering epithelial tissue growth, resulting in prolonged healing times.
Requires secondary fixation, posing a risk of mechanical damage during dressing changes, impacting limb function and aesthetics.
Growth of granulation tissue into the mesh, making it easier for pathogens to penetrate.
Adhesive tape may cause skin allergies, overly tight bandaging affects blood circulation and granulation tissue growth, while loose bandaging can lead to dressing detachment and contamination.
Hydrogel Wound Dressings
In the field of wound care, hydrogel wound dressings emerge as a revolutionary solution, composed primarily of pure water (70%–90%), carboxymethyl cellulose, and other additives. Understanding their mechanisms and applications is pivotal for optimizing their benefits.

Hydrogel wound dressings leverage the natural enzymatic activity present in wound exudate, particularly collagenase, to break down necrotic material. This facilitates autolytic debridement, fostering a self-dissolving wound-cleansing effect.
Applications:
Effective for autolytic debridement in wounds with yellow slough and black necrotic tissue.
Ideal for wounds with low to moderate exudate levels.
Suitable for burns and radiation injuries.
Applicable to wounds exposing bone membranes or tendons.

Advantages:
Hydrates wounds, creating a conducive environment for cell proliferation.
Promotes autolytic debridement, especially beneficial for wounds with necrotic tissue.
Facilitates epithelial migration and granulation tissue growth.
Non-adherent, pain-relieving, and doesn’t damage the wound during dressing changes. It can fill deep wound cavities effectively.
Drawbacks:
Lacks a bacterial barrier.
Prone to causing surrounding skin maceration.
Requires a secondary dressing.
Not suitable for heavily exudating wounds.
The dressing color may turn green, potentially confusing with Pseudomonas aeruginosa infection.
Hydrogel wound dressings, with their unique properties, represent a significant leap forward in wound care technology. Their ability to promote a moist wound environment and facilitate autolytic debridement makes them a valuable asset in accelerating the healing process.
Alginate Wound Dressings
Primarily composed of sodium carboxymethyl cellulose and calcium alginate, alginate dressings undergo ion exchange with wound exudate, transforming into a gel. This gel formation creates a moist healing environment, stimulating cell proliferation, activating macrophages for infection control, and releasing growth factors to expedite healing. The ion exchange also contributes to hemostasis and stabilizes the biological membrane.

Applications:
Ideal for wounds with moderate to high exudate levels.
Suited for wounds with cavities or sinus tracts.
Effective for infected wounds with necrotic tissue.
Applicable to cancerous wounds.
Particularly beneficial for highly exudating chronic wounds, such as pressure ulcers and various ulcers.

Advantages:
High absorbency.
Conforms to wound contours, suitable for both shallow and deep wounds.
Creates a moist environment, promoting cell proliferation.
Maintains nerve endings’ moisture, alleviating pain.
Assists in autolytic debridement by forming hydrogels with necrotic tissue.
Easy to apply and remove, non-toxic, and hypoallergenic.
Drawbacks:
Requires a secondary dressing for fixation.
Unsuitable for dry, minimally exudating, or heavily necrotic wounds.
Difficulty in removing residual dressing in wounds with deep sinuses.
May produce an odor, resembling pus, potentially confusing with wound infection.
Relatively higher cost.
Not suitable for individuals allergic to alginate.
In the world of wound care, alginate dressings emerge as a dynamic solution, ushering in a new era of advanced healing. Their versatility and ability to adapt to various wound types underscore their significance in optimizing the recovery journey.
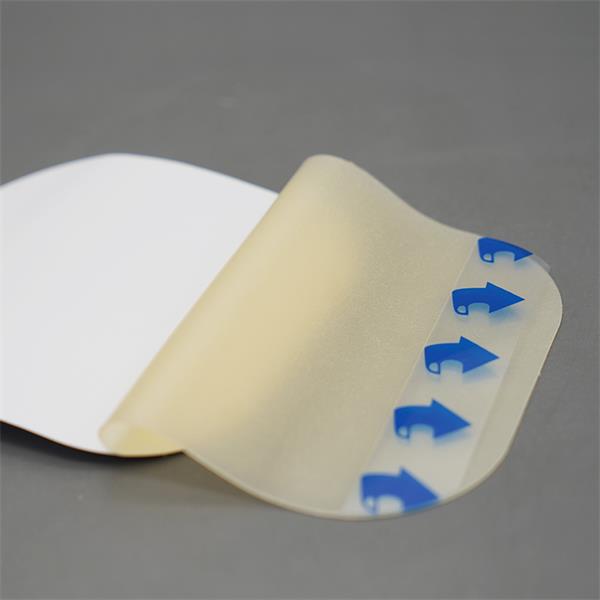
Hydrocolloid Wound Dressings
Primarily composed of flexible polymerized hydrogel, synthetic rubber, and adhesive materials, hydrocolloid wound dressings possess intrinsic enzymes promoting the dissolution of fibrin and necrotic tissue. They activate polymorphonuclear leukocytes and macrophages, effectively facilitating debridement. The dressing’s hydrophilic particles interact with water, forming a gel that creates a moist environment, reduces pain, and does not harm new tissue.

Applications:
Suitable for superficial wounds with partial skin loss.
Effective for wounds with low to moderate exudate levels.
Ideal for burn injuries and surface wounds in soft tissues.
Advantages:
Maintains wound moisture, creating a low-oxygen, slightly acidic environment for accelerated healing.
Softens yellow slough, supporting autolytic debridement.
Absorbs low to moderate exudate, reducing the frequency of dressing changes.
Adhesive nature allows for a sealed wound without the need for a secondary dressing, providing waterproof and antimicrobial properties.
Offers comfort, reduces friction, and acts as a pressure-relief mechanism.
Forms a gel after absorbing exudate, keeping nerve endings moist, and doesn’t adhere to the wound during removal, minimizing pain.
Highly conformable, and easily customizable to fit various wound shapes.

Drawbacks:
Opaque nature limits direct observation of the wound; not recommended for wounds requiring close monitoring.
Unsuitable for infected wounds or those with exposed muscles or bones.
The dressing may have an odor and appear pus-like, leaving a brown residue upon removal.
Not recommended for heavily exudating wounds due to potential overhydration.
Inapplicable to infected wounds.
Risk of damaging fragile surrounding skin during removal; susceptible to softening or deforming under heat and friction.
Hydrocolloid wound dressings redefine wound care with their versatile properties, offering a balance between comfort and efficacy in the healing process. Their application showcases a paradigm shift towards advanced, patient-friendly solutions.
Foam Wound Dressings
Composed of polyurethane and polyethylene alcohol foam, foam dressings boast a porous structure that absorbs substantial exudate, creating a moist, warm, and sealed environment conducive to wound healing. These wound dressings allow almost complete permeability to oxygen and carbon dioxide, making them effective drug carriers.

Applications:
Ideal for wounds with moderate to heavy exudate, such as stage II and III pressure ulcers.
Advantages:
Provides a moist, warm, and sealed environment, supporting autolytic debridement.
Absorbs moderate to heavy exudate, minimizing the impact of exudate and saturation on the wound.
Allows the passage of gases and water vapor, suitable for infected wounds.
User-friendly, highly conformable, easy to remove without causing skin damage, and adaptable to various body parts.
The semi-permeable surface membrane prevents dust and microbes from entering, while the foam pad cushions external pressure, ensuring comfort.

Drawbacks:
Opaque nature impedes direct observation of the wound.
Not suitable for dry wounds, wounds with black necrotic tissue, or eschar.
Limited effectiveness in wounds with minimal exudate.

Case Example:
In the treatment of a pressure injury, following local debridement, an inner layer of silver-ion alginate dressing was applied, secured by an outer layer of foam dressing. This combination effectively absorbed a significant amount of exudate, promoting optimal wound healing conditions.
Silver Ion Wound Dressings
Silver ion wound dressings, a cutting-edge antimicrobial solution, comprise polyurethane foam, sodium carboxymethyl cellulose, and silver. Rapid in bacterial eradication, these dressings continuously release low concentrations of silver ions, showcasing a formidable defense against infections.

Silver ions, carrying a positive charge, exhibit high toxicity to microbes, fungi, and certain viruses, inhibiting their growth. The positive ions interfere with bacterial cell wall protein synthesis, disrupt cell nucleus DNA division, and compromise the synthesis of the bacterial respiratory energy chain, leading to bacterial cell death. The bactericidal effect remains potent for 3 to 7 days.
Applications:
Severely contaminated wounds
Infected wounds
Graft donor sites
Central venous catheter insertion sites
Diabetic foot ulcers
Pressure sores, among others.

Advantages:
Broad-spectrum antimicrobial action with robust infection-fighting capabilities, releasing silver ions continuously for rapid bacterial eradication.
Quick and substantial absorption of exudate, minimizing skin saturation.
Maintains wound moisture, expediting wound healing and reducing scar formation.
Drawbacks:
Not suitable for individuals allergic to silver.
Not recommended for those undergoing magnetic resonance imaging (MRI).
Relatively higher cost.
Silver ion wound dressings stand as a formidable ally in wound care, showcasing their prowess in combating infections and fostering an environment conducive to rapid healing. Their antimicrobial efficacy makes them a valuable asset, particularly in challenging clinical scenarios.
Silicone Foam Wound Dressings
Silicone foam wound dressings, crafted from sterile polyurethane foam infused with silicone adhesive, emerge as a revolutionary solution in wound care. Explore their composition, unique mechanisms, applications, and the remarkable benefits they bring to the forefront of managing various types of wounds.
Comprising sterile polyurethane foam with silicone adhesive, these dressings boast a distinctive 3D tree-like foam structure, facilitating vertical absorption and snug adherence to the wound bed. Their exceptional fluid management capabilities, powered by SAP three-dimensional lock liquid technology, efficiently secure and manage exudate. The surface silicone layer, gentle on the skin, promotes a safe and comfortable fit, while the three-piece non-contact protective film enhances overall wound protection.

Applications:
Suitable for various exudative wounds.
Thin silicone foam dressings are apt for non-exudative/low-exudate wounds.
Particularly beneficial for wounds in areas requiring increased mobility, such as joints.

Advantages:
Exceptional absorption capacity, minimizing the occurrence of saturation and leakage.
Provides an ideal moist wound healing environment.
Offers enhanced protection for the fragile skin surrounding the wound.
User-friendly and easy to apply.
Strikes an optimal balance between excellent absorbency and safe adherence.

Drawbacks:
Relatively higher cost.
Case Example:
Following radiation therapy for post-mastectomy complications, including radiation dermatitis, a breast cancer patient underwent local cleansing with saline solution. Subsequently, a silicone foam dressing was applied and secured, showcasing its efficacy in managing the aftermath of radiation-induced skin issues.
Bioactive Wound Dressings
Discover the transformative impact of bioactive dressings, meticulously crafted from the synergy of Fibroblast Growth Factor (FGF) and collagen protein. Unravel their unique advantages, suitable applications, and essential considerations for optimal wound care.

Advantages:
Proactive Tissue Restoration:
Actively initiates and accelerates tissue repair, reducing scar formation and shortening wound healing duration.
Neurotrophic Effects:
FGF, akin to the Nerve Growth Factor (NGF), supports neuron survival and stimulates growth, promoting neural health.
Effective Hemostasis:
Exhibits excellent hemostatic properties by inducing platelet aggregation upon contact with blood, triggering the release of clotting factors, and facilitating blood clot formation.
Forms a gel layer on the wound surface, contributing to vascular damage sealing.
Indications:
Suitable for wounds with moderate to high exudate levels or wounds with cavities and sinus tracts.
Ideal for wounds with impaired clotting function or those at risk of postoperative bleeding.
Precautions:
Essential to thoroughly clean the wound before application, ensuring infection control.
Incompatible Combinations:
Should not be used in conjunction with ointment antibiotics, alcohol, or iodine solutions.
Bioactive wound dressings emerge as a groundbreaking solution in wound care, harnessing the regenerative potential of FGF and collagen. As a catalyst for active healing, these dressings redefine the trajectory of wound management, offering a promising avenue for enhanced patient outcomes and reduced healing times.
Lipid Hydrocolloid Silver Sulfadiazine Dressings
Explore the cutting-edge features and versatile applications of Lipid Hydrocolloid Silver Sulfadiazine dressings, a revolutionary product combining water colloidal particles, carboxymethyl cellulose sodium, vaseline, and silver salt within a polyurethane mesh.
Advantages:
Conforming to Complex Wounds:
Adapts seamlessly to wound contours, making it suitable for challenging areas.
Protective Skin Barrier:
Safeguards the fragile skin surrounding the wound, allowing for easy customization without adhering to adjacent tissues.
Versatile Applications:
Wide-ranging utility, effective for both wound packing and drainage, and compatible with negative pressure wound therapy.
Broad-Spectrum Antimicrobial Action:
Exhibits prolonged antibacterial activity for up to 7 days, combating a variety of microbes, including MRSA, VRE, and ESBL.
Drawbacks:
Limited Absorption:
Incapable of absorbing exudate, potentially causing peri-wound maceration.
External Dressing Fixation:
Requires additional outer dressings for secure placement.
Indications:
Chronic Wounds:
Effective for pressure injuries and leg ulcers.
Acute Wounds:
Applicable to burns, traumatic injuries, and post-surgical wounds.
These wound dressings mark a significant advancement in wound care, providing a multifaceted solution for intricate wounds. The incorporation of lipid hydrocolloid technology, silver sulfadiazine, and a polyurethane mesh underscores its potential to redefine wound healing outcomes, offering enhanced protection and versatility.
Hypertonic Saline Dressings
Discover the remarkable benefits of Hypertonic Saline Wound Dressings, composed of absorbent polyester fibers and 28% sodium chloride, creating an environment conducive to accelerated wound healing.

Advantages:
Facilitating High Osmolarity Environment:
Creates a high osmolarity environment, promoting the effective removal of bacteria and necrotic tissue.
Versatility in Deep Cavity Wounds:
Suitable for deep cavity wounds such as sinuses, pressure ulcers, and lower extremity ulcers.
Enhanced Tissue Healing:
High permeability reduces tissue edema, stimulates granulation tissue growth, and expedites the local wound healing process.
Drawbacks:
Not Suitable for Intact Skin:
Should not be applied to normal skin, necessitating daily changes.
Indications:
Deep Cavity Wounds:
Ideal for wounds with significant depth, including sinuses, fistulas, and abscess incisions.
Granulation Tissue Edema:
Effective in reducing edema in wounds during the inflammatory and granulation phase.
High-Secretion Wounds:
Appropriate for wounds with substantial exudates, such as pressure ulcers, surgical wounds, diabetic foot ulcers, and lower extremity venous ulcers.
Hypertonic Saline Wound Dressings emerge as a valuable option for wound care, particularly in scenarios where high osmolarity is beneficial. Their versatile application and positive impact on tissue healing make them a promising choice for clinicians aiming to optimize wound management outcomes.
Liquid Wound Dressings
Explore the innovative Liquid Dressings, a synthesis of three polymer compounds primarily composed of high-molecular-weight acrylic acid, alcohol-free for optimal wound care.

Advantages:
Non-Toxic and Alcohol-Free:
Free from toxic components and alcohol, ensuring a painless and non-irritating application that doesn’t impede wound healing.
Rapid Drying and Extended Protection:
Dries in as fast as 30 seconds, providing effective protection for up to 72 hours without the need for frequent reapplication.
Breathable Waterproof Film:
Forms a breathable and waterproof film on the skin’s surface, preventing exposure to moisture from urine, feces, digestive fluids, drainage, etc., reducing friction.

Usage Guidelines:
Preparation for Application:
Clean and dry the skin before use; apply the second layer after the first layer is completely dry.
Application in Skin Folds:
Apply to areas like the inner thighs or buttock folds by gently separating the skin folds for application and releasing after drying.
Reapplication Timing:
Depending on the patient’s condition, reapply every 24-72 hours; avoid simultaneous use with lotions, creams, or ointments.
Applications:
Incontinence-Associated Dermatitis (IAD):
Ideal for skin care in cases of urinary or fecal incontinence.
Stoma and Periwound Care:
Effective in protecting the skin around stomas and wounds.
Diaper Rash in Infants:
Suitable for managing diaper rash in infants and young children.
Liquid Wound Dressings emerge as a user-friendly, durable solution for skin protection in various scenarios, offering a breathable shield without compromising patient comfort.

Key Principles for Dressing Selection
Optimal wound care involves a strategic approach to dressing selection, considering various factors that influence the healing process. Here are essential principles to guide the choice of dressings for different wound scenarios.
Wound Stage Classification:
Evaluate wounds based on their healing stages to align dressing choices with specific needs.
Assessment of Exudate Levels:
Consider the amount of wound exudate, adapting dressings to manage different levels of fluid drainage effectively.
Infection Status:
Determine the presence of infection and choose dressings with antimicrobial properties when necessary.
Odor, Adhesiveness, and Ease of Removal:
Address concerns related to dressing odor, adhesiveness, and ease of removal to enhance patient comfort and compliance.
Skin-Friendly Characteristics:
Select dressings that minimize skin irritation, ensuring optimal absorption and protection.
Frequency of Dressing Changes:
Adjust dressing change schedules based on the wound’s needs, balancing efficiency with patient comfort.
Usability:
Choose dressings that are user-friendly, allowing for easy application and maintenance.
Pain During Dressing Changes:
Consider the pain level associated with dressing changes and opt for solutions that minimize patient discomfort.
Protection of Surrounding Skin:
Prioritize wound dressings that not only aid wound healing but also provide a protective barrier for the surrounding skin.
Patient Preferences:
Incorporate patient preferences into dressing selection when possible to enhance overall satisfaction and compliance.

In clinical practice, the dynamic and individualized nature of wound care demands a flexible and comprehensive approach. By considering these principles and adapting dressing choices to the specific needs of each patient, healthcare providers can achieve the best treatment outcomes. Effective wound care hinges on selecting dressings that are safe, efficient, easy to use, and offer the best value for patients.







