What Is A Hemodialyzer
The “Hemodialyzer” or “Hemodialysis Machine” is a crucial medical device used to perform a life-saving procedure called hemodialysis. Hemodialysis serves as a substitute for the kidney’s natural function of filtering harmful waste and excess fluids from the bloodstream. This process is vital for individuals experiencing acute kidney failure, end-stage renal disease (commonly known as uremia), and cases of drug poisoning where the kidneys are unable to effectively perform these functions.
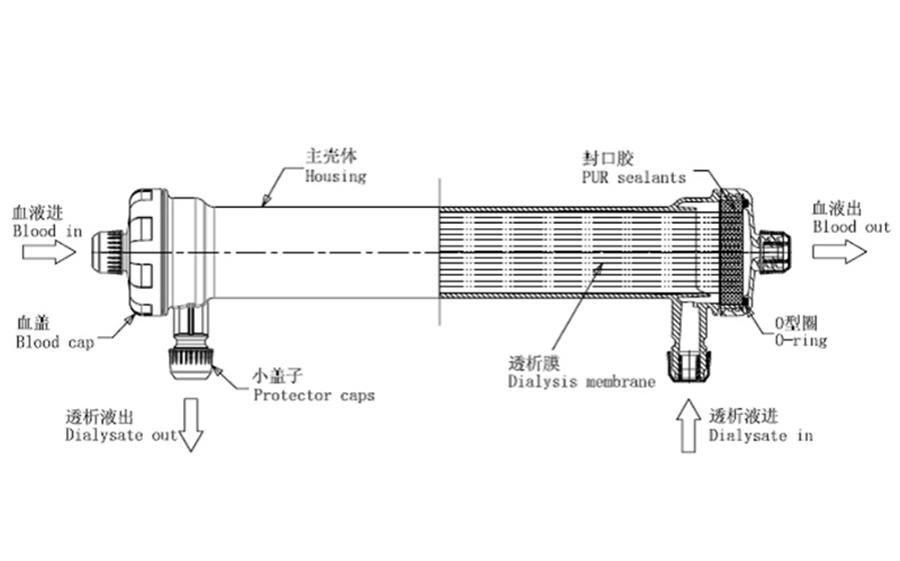
During hemodialysis, a patient’s blood is safely diverted through the hemodialyzer, which contains a specialized filter known as a dialyzer. This dialyzer helps remove waste products, toxins, and excess fluids from the blood, which the compromised kidneys cannot eliminate on their own.

Product Overview:
Disposable Medical Hemodialyzer
Material: PES
Disinfecting Type: ETO
Size: 1.4㎡,1.6㎡,1.8㎡,2.0㎡;
Model: Low Flux and High Flux
Application: Hospital Hemodialysis



Low Flux 1.4/1.6/1.8/2.0 m2
4. Lower loss of Albumin
2. Lower resistance membrane
3. Higher permeability for middle to large-size molecules
4. Excellent blood compatibility
Get Solution
Types of Medical Hemodialyzer
Ultrafiltration Coefficient Classification:
High Flux Hemodialyzers:
These hemodialyzers feature an average pore size of 2.9nm (nanometers) with a maximum diameter of 3.5nm. Composed of hydrophobic groups and different hydrophilic components, they exhibit excellent diffusion and ultrafiltration capabilities. High flux hemodialyzers typically have an ultrafiltration coefficient equal to or greater than 20 ml/(mmHg·h), urea clearance rates of 185-192 ml/min, creatinine clearance rates of 172-180 ml/min, vitamin B12 clearance rates of 118-135 ml/min, and a β2-MG sieving coefficient greater than 0.65.
Low Flux Hemodialyzers:
These hemodialyzers have an average pore size of 1.3nm with a maximum diameter of 2.5nm. They are highly hydrophilic and excel at removing small molecular toxins. Typically, low flux hemodialyzers have an ultrafiltration coefficient ranging from 4.2 to 8.0 ml/(mmHg·h), urea clearance rates of 180-190 ml/min, creatinine clearance rates of 160-172 ml/min, vitamin B12 clearance rates of 60-80 ml/min, and minimal clearance of β2-MG.

Membrane Material Classification:
Unmodified Cellulose Membranes:
These membranes are derived from natural cellulose fibers dissolved and regenerated. They possess high hydrophilicity and permeability but exhibit poor biocompatibility. Their clearance abilities for medium to large molecular toxins (e.g., cuprophane and cellulose acetate membranes) are limited.
Modified or Regenerated Cellulose Membranes:
These are cellulose membrane derivatives with various substituent groups attached to the cellulose backbone. They excel at clearing small molecules and phosphates, making them efficient dialyzer materials. However, their blood compatibility still requires improvement (e.g., hemophane and cellulose triacetate membranes).
Synthetic Membranes:
Typically asymmetric hydrophobic membranes, have a wide range of relative molecular weight cut-offs. They offer higher ultrafiltration coefficients and better biocompatibility. Synthetic membranes can be stretched to achieve various pore sizes (e.g., polysulfone and polyethersulfone membranes).

How Does Medical Hemodialysis Work?
Medical Hemodialysis is one of the treatment methods for patients with acute or chronic kidney failure. It works by diverting the patient’s blood from their body, passing it through a dialyzer composed of numerous hollow fibers. Within this dialyzer, the blood comes into contact with an electrolyte solution called dialysate, which has a composition similar to that of the body’s fluids.
Through a process known as diffusion, substances are exchanged between the blood and the dialysate within these hollow fibers. This exchange helps remove metabolic waste products, maintain electrolyte balance, and regulate acid-base levels in the body.
Additionally, hemodialysis aids in removing excess fluid from the body, and the purified blood is then returned to the patient’s circulation. The entire process of diverting, purifying, and returning the blood is referred to as hemodialysis.


The Key Terminology in Medical Hemodialysis
Ultrafiltration Coefficient (Kuf):
The ultrafiltration coefficient, denoted as Kuf, represents the volume of fluid transported across a membrane per hour, per millimeter of mercury (mmHg) pressure gradient. It serves as a measure of the dialyzer’s ability to allow the passage of water. A higher Kuf indicates greater permeability to water, meaning it can efficiently remove excess fluid during hemodialysis.
Low-Flux Dialysis:
Low-flux dialysis refers to the hemodialysis process conducted using low-flux dialyzers. These dialyzers are characterized by having an ultrafiltration coefficient (Kuf) of ≤10 ml/(mmHg·h). They are designed for specific patient needs where minimal solute removal is required.
High-Flux Dialysis:
Conversely, high-flux dialysis involves the use of high-flux dialyzers in combination with ultrapure dialysate during hemodialysis. High-flux dialyzers possess an ultrafiltration coefficient (Kuf) of ≥20 ml/(mmHg·h), making them efficient in clearing a broad range of solutes.
Hemofiltration:
Hemofiltration mimics the natural function of renal glomeruli by utilizing high-flux dialyzers and replacement fluid. It primarily employs a convection-based mechanism to remove toxins from the bloodstream.
Hemodiafiltration:
In hemodiafiltration, high-flux dialyzers are employed in tandem with a combination of diffusion and convection principles. This dual-action approach effectively clears toxins from the blood during the purification process.
Hemoperfusion:
Hemoperfusion involves diverting a patient’s blood from their body and passing it through an adsorber within a perfusion device. This method relies on adsorption to eliminate toxins, drugs, and metabolic waste products from the bloodstream.
OUR COMPANY
Why Choose Us
With over two decades of expertise in the field of medical consumables, a vast portfolio comprising more than 1000 healthcare products, and a global presence spanning over 100 countries, our company, JINYE, stands as a seasoned and reliable partner in the healthcare industry.




Common Questions
Most Popular Questions.
Frequently Asked Questions (FAQ) about Medical Hemodialyzer and Hemodialysis Knowledge
Hemodialysis is necessary when the kidneys cannot adequately remove waste and excess fluid from the body.
Blood is drawn from the patient, passed through a hemodialyzer, filtered, and then returned to the patient's body.
Dialysate is a fluid used in hemodialysis to help remove waste and maintain electrolyte balance in the blood.
Complications can include low blood pressure, infection, muscle cramps, and anemia.
Hemodialysis filters blood externally, while peritoneal dialysis uses the abdominal lining to filter waste internally.
Kidney transplantation is an alternative, but not everyone is a suitable candidate.
Symptoms include fatigue, swelling, nausea, and difficulty concentrating. Lab tests confirm the need for hemodialysis.
Hemodialysis itself is not painful, but some patients may experience minor discomfort at the needle insertion site.
Hemodialyzers are single-use devices and should be replaced after each session to prevent infection and maintain effectiveness.
The Kt/V and URR (Urea Reduction Ratio) are common measures of dialysis adequacy.
Hemodialyzer
We would love to hear from you.
Get in touch
Leave us a message
To Get The Latest Medical Consumables Solutions
16 Evaluation Indicators for Hemodialyzers
Compliance:
Compliance in hollow fiber membranes refers to the need for blood chambers not to expand excessively to prevent increased extracorporeal blood volume.
Residual Blood Volume:
After rinsing with 200 ml of saline at the end of dialysis, the residual blood volume within the dialyzer should ideally be minimal, usually less than 1.0 ml.
Membrane Adsorption:
Synthetic membranes have a notable adsorption capacity, allowing them to adsorb proteins from the blood, such as small molecular proteins (β2-MG) and certain therapeutic drugs like erythropoietin, serving both biological and clinical purposes.
Blood Flow Resistance:
Hollow fiber dialyzers may have different internal resistances, with membrane resistance being higher than that of flat plate dialyzers. Typically, resistance should be below 20 mmHg (blood flow rate of 200 ml/min) to avoid increased arterial pressure.
Ultrafiltration Coefficient (Kuf):
Kuf measures the overall ultrafiltration capacity of a specific dialyzer. It represents the volume of liquid that can cross the membrane per hour under a pressure gradient of 1 mmHg. Kuf reflects the membrane’s permeability and is influenced by factors such as pore size, thickness, and surface area.
Anticoagulant Properties:
Some membranes can combine with heparin or other anticoagulants, reducing the required heparin dosage and preventing complications associated with long-term heparin use. Currently, there are no heparin-free dialyzer membranes, but polyethylene vinyl alcohol membranes may reduce heparin usage or be suitable for heparin-free dialysis.
Dialyzer Membrane Material:
Dialyzer membranes are primarily made from cellulose, modified cellulose, or synthetic materials, each with its unique characteristics.
Membrane Surface Area:
The dialyzer’s surface area is related to its clearance rate and ultrafiltration coefficient. However, surface area doesn’t always correlate directly with urea clearance rates.
Clearance Rate:
Clearance rate and ultrafiltration rate are two crucial functions of a dialyzer, serving as key indicators of its quality. Commonly used indicators for evaluating clearance rates include urea, creatinine, vitamin B12, and β2-MG.
Biocompatibility:
Dialyzer biocompatibility primarily involves its reaction with blood, often leading to complement activation. Enhancing blood/membrane biocompatibility is crucial for improving dialysis quality and minimizing complications.
Membrane Hydrophilicity:
The hydrophilicity of a dialyzer membrane depends on its chemical composition and how it interacts with water. For instance, cellulose and polyethylene vinyl alcohol membranes exhibit strong hydrophilicity, while polymethyl methacrylate and polyamide have lower hydrophilicity.
Membrane Permeability:
Dialyzer membranes should withstand moderate pressure, typically up to 500 mmHg during dialysis, without membrane rupture.
Pre-Blood Volume:
The pre-blood volume within the dialyzer should be moderate, typically ranging from 60 to 80 ml for adult dialyzers. An excessively large pre-blood volume can increase extracorporeal blood volume and potentially cause low blood pressure.
Disinfection Methods:
Dialyzers are typically disinfected using one of three methods: ethylene oxide (ETO), gamma radiation, or high-pressure steam (wet or dry). High-pressure steam disinfection is less harmful to humans, but some synthetic membranes may not tolerate it, making ETO the widely used disinfectant.
Reusability Rate:
Ensuring the quality of reused dialyzers is critical. Proper rinsing, purification, and disinfection procedures should be followed. A common benchmark for reused dialyzers is to discard them if capacity decreases by 15% or if the ultrafiltration rate drops by 25%.
Quality-to-Price Ratio:
Dialyzers that offer satisfactory clearance rates, ultrafiltration rates, and reusability, while maintaining affordability, are considered to have a favorable quality-to-price ratio.


